NAUSEA AND VOMITING
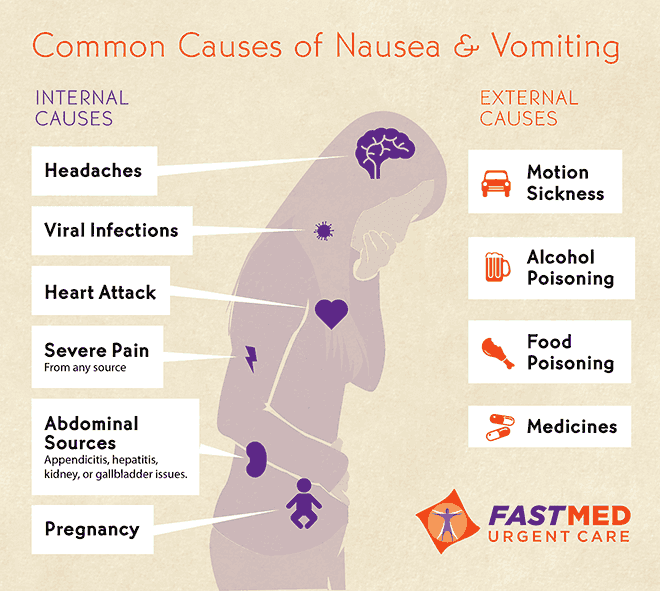
Consider the underlying mechanisms and potential causes:
-establish the history (when and how did it start, other symptoms or illnesses, pain, has it happened before, anyone else got the same symptoms?).
-is this gastrointestinal disease (any diarrhoea, abdominal pain, obstruction, is the cause acute liver damage, alcohol abuse?)
-is it drug-related? (any new medication, digoxin toxicity or opiate side-effect?)
-could this be raised intracranial pressure? (headache, malignant disease or altered consciousness level?)
-could this be metabolic? (renal failure, sodium and calcium levels, ketoacidosis?).
Nausea and vomiting in acute medical conditions:
-Migraine: commonly accompanied by vomiting. Other causes of headache like meningitis, increased intracranial pressure and subarachnoid haemorrhage are also associated with vomiting.
-Myocardial infarction: vomiting is an important feature that distinguishes the pain of a myocardial infarction from that of angina and is often accompanied by nausea and sweating.
-Sepsis: vomiting can be the only symptom of hidden infection, particularly in infections in the kidneys and lower urinary tract.
-Acute gastric dilatation: gross gastric distension leads to upper abdominal swelling associated with nausea, often accompanied by hiccups and belching. A common outcome is sudden vomiting, aspiration an cardiac arrest.
ACUTE UPPER GASTROINTESTINAL HAEMORRHAGE
Causes:
-Helicobacter pylori infection and bleeding peptic ulcers
-Acute gastritis, duodenitis and acute erosions (stress ulcers)
-Mallory-Weiss tear:
-Oesophageal varices
-Gastric and oesophageal cancer
-Dieulafoy´s erosion: erosion of a congenitally abnormal artery in the lining of the stomach, emergecy surgery is often required.
Management:
-Ensuring the safety of the patient: ABCDE.
-Investigations: endoscopy.
-Assessing the degree of bleeding: history (presence of melaena with haematemesis, clots in the vomit and recognisable blood in the stool, bleeding accompanied by syncope, postural dizziness and overwhelming thirst suggest a major bleed) and examination (pale and clammy, tachycardia of more than 100 beats/min , systolic blood pressure of less than 100mmHg and postural hypotension).
-Risk assessment with the Rockall Score:
Important nursing tasks:
-ensure the safety of the patient, assess the likely severity of the initial blood loss and report any further loss, save any important evidence (vomited blood, fresh melaena), report any abdominal pain.
-correct the oxygen saturation,
-secure the venous access and ensure accurate fluid balance charts,
-complete baseline observations, measure the pulse, blood pressure and respiratory rate. Report any changes on vital signs which should be checked at appropiate intervals.
-identify the signs of shock (pallor, sweating, restlessness, confusion),
-take an appropiate history, ask about liver disease and clotting disorders,
-reassure the patient and attend to patient´s basic comforts, warn about the likely need for an endoscopy.
ACUTE LIVER FAILURE AND HEPATIC ENCEPHALOPATHY
Acute liver failure can be precipitated by an acute event such as viral hepatitis or by a background of chronic liver disease with portal hypertension.
Components of acute liver failure:
-impairment of the consciousness level: the combination of poor liver function and portosystemic shunting means that toxic substances are either dealt with ineffectively by the liver or bypass it altogether. The result is a toxic encephalopathy with imapirment of the consciousness level that can progress rapidly from confusion and agitation to deep coma. It is useful to assess and follow changes using the Hepatic encephalopathy scoring system:
-bleeding varices and clotting abnormalities: patients in acute liver failure are at great risk from upper gastrointestinal bleeding due to the combination of varices and impaired clotting.
-sepsis: infection can trigger or complicate acute liver failure.
-metabolic abnormalities: the main problems are hypoglycaemia and renal failure.
Critical nursing tasks in acute liver failure:
-Ensure the safety of the patient: ABCDE.
-Gain venous access.
-Carry out top-to-toe examination.
-Liaise with patient´s family.
-Ascertain the possible causes of acute liver failure: the most common are paracetamol poisoning and acute hepatitis.
-Explain the likely interventions in the first 48 h: endoscopy, radiology, transfusions, multiple infusion lines and possible transfers.
-Obtain a drug history.
Other important nursing tasks are: determine accurate fluid balance, identify sepsis, reassure the patient and manage confusion and disorientation, carry out general nursing measures.
ACUTE ABDOMINAL PAIN
Abdominal pain is a common complaint on the acute medical ward and it is a feature of several medical conditions.
Nursing tasks:
-Establish the site and pattern of the pain.
-Assess the severity of the pain.
-Look for signs of shock (tachycardia, hypotension and increased respiratory rate).
-Examine for abdominal rigidity and peritonitis: the most obvious features of acute peritonitis are localised pain on coughing and board-like abdominal rigidity, the patient does not want to move, appears shocked and is usually vomiting. Acute peritonitis may be accompanied by signs of sepsis (hypotension, rapid thready pulse and cold, mottled extremities).
-Prepare for resuscitation: the basic requirements are oxygen, IV fluids, nasogastric intubation and urinary catheterisation.
Also, it is important to look at associated clinical features, prepare the patient for further investigations, review the previous history, the urine test results and the stool chart.
ACUTE DIARRHOEA
Infective diarrhoea:
Assessment:
-History of recent foreign travel
-Ask about other possible cases
-Have there been recent doubtful meals/mass catering...?)
-History of recent antibiotic therapy
-Is this patient at special risk?: elderly, diabetic, immunosuppressed, cardiac and kidney disease.
-Is there a history of recurrent diarrhoea?: inflammatory bowel disease.
Nursing assessment: ABCDE, assess fluid loss, look for evidence of shock and diagnosis from stool cultures.
-Infection control.
-Correct fluid deficit and keep up with the loss of fluid in the stool and vomit (fluid balance and stool chart).
-Antibiotics are rarely needed unless there are signs of complications: persistent fever with a failure to improve, development of severe colitis or shock, signs of infection, severe colitis with the risk of haemorrhage, toxic dilatation and perforation or HUS (Haemolytic Uraemic Syndrome).
Clostridium Difficile diarrhoea
The indiscriminate use of antibiotics has led to a large rise in bowel infections due to clostridium difficile. The clinical picture varies from mild diarrhoea to severe colitis with fever, systemic sepsis and death.
Diagnosis relies on two fresh stool specimens from any patient with mushy or liquid stools beng sent urgently to the labwith a request for the C.difficile toxin. The result should be available on the same day. Specific treatment is with oral metronidazole or vancomycin.
The following indicate a potentially severe infection:
-Temperature > 38.5
-More than 7 episodes of diarrhoea per 24 hours
-Pulse > 100
-WCC > 15 x 109
-A 50% rise in initial creatinine level (developing renal failure)
-Distended abdomen and no diarrhoea.
C. difficile and its spores contaminate and survive on surfaces such as commodes and bedside equipment and, in a busy ward , are easily spread by staff from one patient to another.
Enteric precautions: a single room with an en-suite commode, staff wearing gloves and apron who wash their hands with soap and water before entering and leaving the room, liquid soap and disposable wipes for the patient.
Source:






No hay comentarios:
Publicar un comentario